The hidden allies of cancer
How spatial omics is bringing normal cell interactions into focus
In cancer, even the normal cells can become key players, sometimes helping the tumor instead of fighting it.
While we usually think of these cells as defenders against cancer, tumors can manipulate them to support their growth. Spatial omics technologies are helping us understand how this happens, and these discoveries are not just academic. They are laying the groundwork for more precise and effective cancer therapies.
In the end, the future of cancer treatment may lie in targeting the interactions between these apparently benevolent cells.
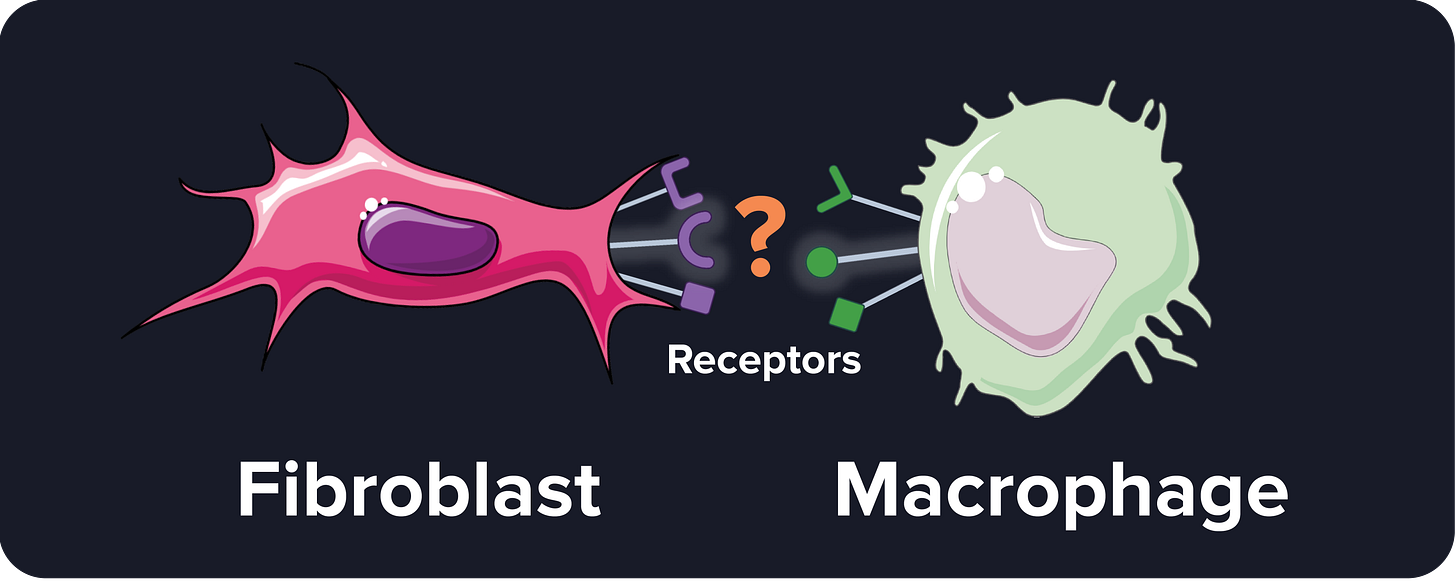
Background: the fibroblast-macrophage connection
Scientists have long suspected that two types of normal cells might collaborate to support the tumor: fibroblasts and macrophages. What is their role in normal conditions?
Fibroblasts help repair wounds by producing collagen and other fibers that form the scaffold of tissues, known as extracellular matrix.
Macrophages are the body's janitors, capable of digesting pathogens, cell debris, and other foreign materials through a process called phagocytosis.
Tumors that have both fibroblasts and macrophages generally lead to worse survival rates compared to tumors with just one of these cell types.
Before spatial omics, these observations would come from counting the number of fibroblasts and macrophages in tumors and observing the progression of cancer, without understanding their spatial interactions or dynamics.
Without interaction information, most therapies were developed to target only a single cell type rather than trying to disrupt the interaction between multiple ones.
The Sibrotuzumab Case Study
Since fibroblasts and macrophages seemed to be helping tumors grow, it made sense for early clinical trials to target these cells individually. For example, Sibrotuzumab is a drug that targets FAP, a protein present in tumor fibroblasts but rare in normal tissues. In the case of a wound, the FAP protein can break the extracellular matrix and allow the arrival of immune cells to the site, but cancer cells can exploit FAP+ fibroblasts to spread more easily or develop more vasculature to feed the tumor.
However, phase 1 and 2 clinical trials of Sibrotuzumab in humans failed to show a reduction in tumor growth12. The failure of Sibrotuzumab in clinical trials raised questions, and researchers have proposed a few explanations:
FAP is still active: even though Sibrotuzumab binds to FAP, FAP may still be able to degrade the extracellular matrix. How is that possible? Sibrotuzumab may bind to a region of the FAP protein that is not involved in remodeling the extracellular matrix.
No killing ability: antibodies can induce an immune response towards the cells they bind to. However, Sibrotuzumab was not designed to provoke this response.
Cell plasticity: fibroblasts are highly adaptive. It’s possible that targeting FAP induced fibroblasts into deactivating FAP but activating other proteins with similar functions.
Marker vs cause: the tumor growth linked to FAP fibroblasts isn’t directly caused by FAP itself. Instead, while FAP could be used to identify these dangerous fibroblasts, other properties of the cells may be the ones responsible for the tumor growth, such as interactions with different cell types.
What do you think could be other reasons behind Sibrotuzumab's failure? Share your thoughts in the comments, I’d love to discuss them!
Advancements from Spatial Omics
When I first started my PhD, I hadn’t yet heard about the potential interaction between fibroblasts and macrophages. However, from 2022 on, when spatial omics started to pick up steam, these two cell types kept appearing together in study after study345.
All these studies noticed that fibroblasts and macrophages are not only present in the same tumor but are also localized in the same areas.
Not an obvious conclusion, as we saw in the previous blog post.
And that’s not all.
As we will see in the rest of the blog post, thanks to spatial omics, we now have new ideas about what is happening between these cells.
Advancement one: what’s happening inside the tumor?
A recent study6 discovered the dynamics between fibroblasts and macrophages in these tumors. The authors gave immunotherapy to liver cancer patients and classified the patients into two groups: responders and non-responders.
In non-responders, fibroblasts and macrophages form a barrier around the tumor. This barrier acts like a shield, preventing immune cells, specifically T cells, from entering the tumor core and attacking the cancer cells.
This could explain why Sibrotuzumab failed. Even if Sibrotuzumab managed to disrupt the barrier, it’s still not guaranteed that T cells can enter the tumor core, simply because some patients may not have a strong immune response in the first place.
Combining Sibrotuzumab with immunotherapy could help the non-responders break the barrier and bring T cells to the tumor. Still, no one has tested this hypothesis as far as I know.
Advancement two: how are they communicating?
Some studies started to identify the molecules involved in the interaction between fibroblasts and macrophages. For example, by looking at which of the 20,000 genes are active whenever these two types of cells are near each other.
This opens up many possibilities for new cancer therapies. Since they are based on combinations of cell types, they have higher specificity, meaning fewer side effects.
Advancement three: easier to detect
During my master’s thesis, I explored a computational approach called Graph Neural Networks but never had the chance to use it. When I transitioned to my PhD, I decided to work on finding cell communities from spatial omics mainly because they were the perfect use case for Graph Neural Networks.
Spoiler alert: I didn’t use Graph Neural Networks in my PhD either. But this is a story for future blog posts.
Anyway, the more time I spent developing a method to find cell communities, called CellCharter, the more I realized its clinical applicability. Structures like the fibroblast-macrophage barrier are indeed communities and tools like mine could easily detect them.
This means that it could be used to find new potential cancer targets and to assign the right treatment to patients based on the presence or absence of certain interactions.